In 2024, the CDC reported that the U.S. fertility rate was 1.6 children per woman, well below the 2.1 births needed for population replacement. At the same time, births among women over 40 have nearly tripled in the past three decades, reflecting a demographic shift: Americans are waiting longer than ever to start their families.
Social changes, career planning, and medical advances all contribute to later parenthood. But biology still plays a central role, and for many, IVF is the only option when natural conception becomes difficult. That raises a crucial question: How old is too old for IVF?
This guide explores that issue from a medical and technological perspective. We’ll examine how age affects fertility and IVF success rates, as well as strategies that can improve outcomes in later reproductive years.
What is the age limit for IVF treatment?
There’s no universal age limit for IVF. Successful pregnancies have been reported in women well into their 50s. Still, many fertility clinics set an upper age limit between 42 and 45 for women using their own eggs.
The reasons are biological and medical:
Egg quality: As women reach their 40s, the proportion of eggs with chromosomal abnormalities rises sharply. This makes conception harder and increases the risk of miscarriage or genetic disorders.
Menopause: Women who no longer ovulate can’t produce their own eggs for IVF. In these cases, donor eggs or previously frozen eggs are valid options.
Maternal health: Even if conception is possible, pregnancy later in life carries higher risks, including preeclampsia, gestational diabetes, preterm birth, and complications during delivery.
IVF with a woman’s own eggs is rarely recommended beyond age 43. Reproductive specialists generally advise using donor eggs, which offer higher success rates at that point.
If a woman is healthy enough for pregnancy and has access to viable eggs, IVF is possible. As long as the uterus can carry a pregnancy safely, clinics may treat women in their late 40s or early 50s, either with donor eggs or previously frozen eggs.

Source: Amina Filkins
Is there a maximum age for IVF with donor eggs?
There is no legal age limit in the U.S. for IVF with donor eggs, though individual clinics set their own policies. Some extend treatment up to the early 50s, while others set a stricter limit.
About 12% of all IVF cycles in the U.S. use donor eggs. Unlike IVF with your own eggs, where success rates plummet after the early 40s, studies show that the chances of success with donor eggs don’t diminish in your 40s or even 50s. That’s because IVF outcomes depend more on the age of the donor than the age of the pregnancy carrier.
Generally, women over 45 should undergo thorough medical testing to ensure they are physically fit for pregnancy, including screening for cardiovascular and metabolic health.

Source: Antoni Shkraba Studio
What is the best age for IVF?
While there isn’t a one-size-fits-all answer, research and IVF success rates per age are clear: the earlier you pursue IVF, the higher your chances of success.
In general, the optimal age for IVF for women is 35 or younger, which is when egg quality and ovarian reserve are strongest. Older women are also more likely to face fertility-impacting health conditions, such as fibroids or endometriosis.
Male age is also an important, but often overlooked, factor. Studies show that with each passing year, men pass on up to two new genetic variations to their children. Advanced paternal age is linked to a higher risk of conditions such as:
Schizophrenia
Bipolar disorder
Paediatric leukemia

Source: Antoni Shkraba Studio
How age affects fertility
The main biological processes behind the age-related fertility decline are:
The ovarian reserve trajectory
Mechanisms behind egg aging
Uterine receptivity and endometrial factors
Menopause and hormonal changes
1. The ovarian reserve trajectory
Women are born with a fixed number of eggs, called non-growing follicles (NGFs). This reserve declines from birth until menopause. By the age of 30, most women have only about 12% of their original egg supply left, and by 40, this number drops to around 3%.
This decline is known as diminished ovarian reserve (DOR). DOR doesn’t mean that pregnancy is impossible, but it lowers the odds, even with fertility treatments.
At the initial fertility appointment, doctors assess ovarian reserve through blood tests (Anti-Müllerian hormone, or AMH, follicle-stimulating hormone, or FSH, and estradiol) and ultrasound follicle counts. These tests give clues about egg quantity, though none can predict fertility with perfect accuracy.
2. Mechanisms behind egg aging
As eggs age, they undergo biological changes that make fertilization and healthy embryo development more difficult. Some of the most important mechanisms include:
Aneuploidy or chromosomal errors: Older eggs are more likely to have too many or too few chromosomes, which raises the risk of miscarriage and genetic disorders, such as Down syndrome or Turner syndrome.
Mitochondrial decline: Mitochondria are the energy centers of the egg cell. With age, their number and efficiency drop, leaving eggs less capable of supporting embryo development.
DNA damage: Oxidative stress and other aging processes increase the risk of errors in cell division, leading to potential mutations.
3. Uterine receptivity and endometrial factors
Unlike the ovaries, the uterus doesn’t experience such a steep decline in health with age. That’s why older women can still carry pregnancies successfully when younger donor eggs or frozen eggs are used.
Still, research suggests that the endometrium (uterine lining) isn’t entirely immune to aging. Changes occur at the molecular and cellular level, such as:
Cellular senescence: Cells lose their ability to divide and function normally, which may affect implantation.
Inflammaging: Chronic, low-grade inflammation can interfere with embryo implantation and development.
Epigenetic changes: The biological age of endometrial tissue may advance more rapidly than the woman’s chronological age due to chronic inflammation, oxidative stress, and natural cellular wear and tear. These changes can disrupt normal endometrial function.
4. Menopause and hormonal changes
Menopause marks the permanent end of fertility (usually around age 45–51), but the hormonal shifts that lead to menopause start years earlier, narrowing the window of natural conception.
During perimenopause, which typically starts in the 40s, hormones like estrogen and progesterone fluctuate, leading to irregular ovulation. FSH increases as the ovaries become less responsive, signaling reduced fertility.
Even before menopause, egg quality and hormonal patterns make conception more complicated. And while hormonal medications can stimulate the ovaries during IVF, the underlying biological limits of aging eggs still apply.

Source: Amina Filkins
How medical and technological advancements increase IVF age limits
Advances in reproductive technology make it possible for many people to have children later than their natural fertility window. Besides using donor eggs, other options include:
Egg or embryo freezing (cryopreservation)
Optimized IVF protocols
1. Egg or embryo freezing
Freezing eggs at a younger age preserves their quality and genetic integrity, allowing them to be used years later. That is especially valuable for women and couples who are not ready to conceive in their 20s or early 30s but want to preserve their chances of having a biologically related child.
Modern vitrification techniques (quick freezing) have significantly improved survival rates of thawed eggs to up to 99%. And IVF success depends on the age at which eggs are frozen, not the age at which they are used.
Alternatively, women who have a partner or who wish to use donor sperm can freeze embryos created through IVF for future use.
2. Optimized IVF protocols
As fertility declines, standard IVF approaches may not be sufficient.
Older women often require higher doses of fertility medications to stimulate the ovaries and produce multiple high-quality eggs.
Some clinics recommend early egg retrieval and in vitro maturation (IVM) as a treatment option. Research shows that eggs retrieved from older women are sometimes overmature, which reduces fertilization potential.
Early retrieval techniques enable immature eggs to mature in the laboratory, potentially improving egg yield.
What not to do
Many clinics offer so-called mini-IVF or natural-cycle IVF, which uses lower fertility medication doses. The goal is to produce fewer eggs but potentially higher-quality ones, at a lower cost, with fewer injections and side effects.
However, for women over 40 or those with DOR, this approach can reduce the chances of success due to fewer eggs retrieved. Older women already have fewer viable eggs, so producing only one to three per cycle can drastically limit the chance of creating a healthy embryo.
Medical literature doesn’t support the claim that mini-IVF increases egg quality. In fact, studies show that long stimulation protocols can achieve pregnancy rates as high as 48% in women over 35, compared to antagonist or microdose flare protocols.

Source: Mart Production
3. Preimplantation genetic testing
While age-related changes in eggs are unavoidable, there are ways to increase the chances of a successful IVF pregnancy. One of the most effective tools is preimplantation genetic testing (PGT), which screens embryos before transfer to identify those with the best potential for implantation and healthy development.
The available PGT options are:
PGT type | What it detects |
|---|---|
Aneuploidy (extra or missing chromosomes), which becomes more common with age | |
Specific inherited genetic disorders, such as cystic fibrosis, sickle cell anemia, hemophilia, muscular dystrophy, and Tay-Sachs disease | |
Chromosomal structural rearrangements, such as translocations and inversions, which may affect embryo viability | |
Risk for chronic, late-onset conditions, like diabetes or heart disease, impacted by multiple genes, lifestyle, and environmental factors |
Bonus read: Compare different IVF embryo screening options in our guides:
4. IVF surrogacy
For some women, carrying a pregnancy later in life may pose medical risks due to age-related health conditions. In that case, IVF surrogacy or gestational surrogacy offers a safe and effective alternative, allowing couples and single parents to have a biologically related child.
A gestational surrogate is a woman who carries an embryo created via IVF for another individual or couple. The surrogate has no genetic link to the child, and the embryo can be made using the intended parents’ eggs and sperm sample, donor eggs, or donor sperm.
IVF surrogacy is usually recommended when uterine or general health factors make pregnancy risky or impossible. It is also an excellent option for gay male couples.

Source: Ivan Samkov
How age affects IVF success rates
Check out IVF success rates when using your own eggs vs. donor eggs or embryos according to the CDC data from 2022:
Age group | IVF with own eggs | IVF with donor eggs |
|---|---|---|
Under 35 | 42.8% | Up to 45.6% |
35–37 | 39.9% | Up to 41.9% |
38–40 | 43.9% | Up to 43% |
40–45 | 27.7% | Up to 41.7% |
45+ | 10.4% | About 37% |
Success increasingly depends on several key points:
Laboratory expertise
Genetic screening of embryos
Personalized treatment protocols
Expert guidance and informed decision-making
Many clinics may underdeliver on one or more of these factors, particularly for older parents whose fertility potential is already reduced.
A platform like Nucleus IVF+ can make a real difference, combining advanced genetic testing, data-driven embryo analysis, and personalized care and guidance. With its comprehensive approach to IVF, Nucleus helps maximize the chances of a successful pregnancy, even when age-related factors impose additional challenges.

Nucleus IVF+: The smartest start to life
Nucleus doesn’t believe in one-size-fits-all solutions but in choice, transparency, and agency, especially when it comes to growing your family.
Nucleus IVF+ offers an all-inclusive, personalized approach, combining cutting-edge technology and clinical expertise at every step of IVF. It’s built for parents who want to give their children the best possible start in life.
Here’s what Nucleus IVF+ includes:
Clinic matching and tailored IVF cycles: Access an exclusive network of leading clinics with proven success rates.
Comprehensive carrier screening with Nucleus Preview: Get screened for over 2,000 genetic conditions you could pass on to your child.
Tailored guidance 24/7: Receive advice based on your reproductive history, ovarian reserve, age, and medical needs.
Donor matching: Select a genetically compatible donor egg to achieve a healthy embryo and a successful pregnancy.
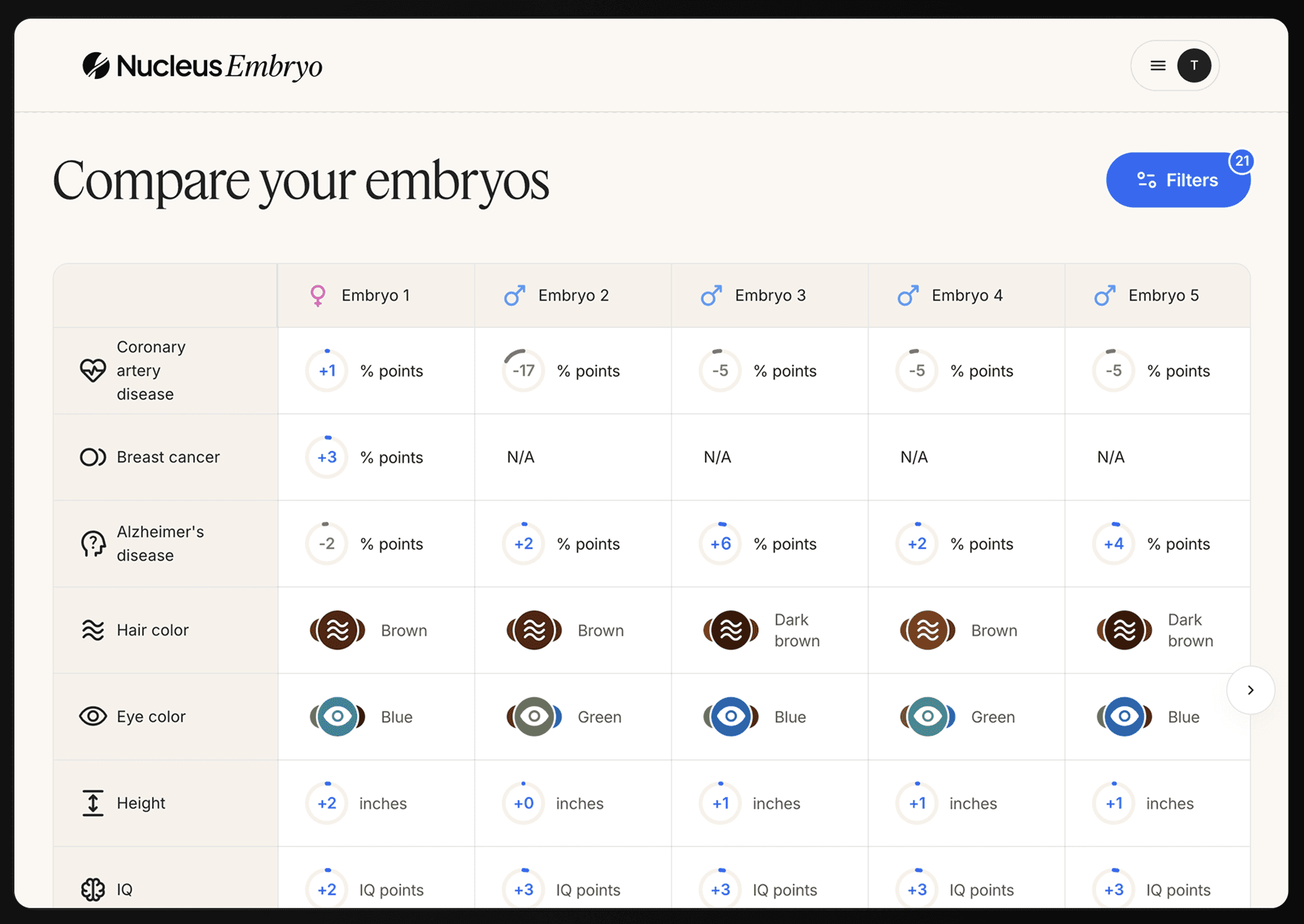
Deep and comparable embryo analysis: Leverage technology to identify embryos with the highest potential for implantation, development, and long-term health through advanced PGT screening.
Health insights for you: Learn more about your genetic status and hereditary risks and get actionable advice so you can improve your longevity outcomes.
Book an onboarding call with the Nucleus team to get started.
You may also like…
Featured image source: Amina Filkins












