Endometriosis is a condition in which tissue similar to the uterine lining grows outside the uterus, often causing pain, inflammation, and in many cases, difficulty conceiving. Since in vitro fertilization helps many potential parents overcome their fertility issues, a common question is: Can you do IVF with endometriosis?
This guide explains whether endometriosis affects IVF success, what the process entails for individuals with this diagnosis, and whether IVF can cause or exacerbate the condition.
Can you do IVF if you have endometriosis?
IVF can be particularly effective for women with endometriosis. The process involves ovarian stimulation to encourage egg maturation, egg retrieval from the ovaries, and fertilization in the laboratory. The resulting embryos are then transferred directly into the uterus, overcoming fallopian tube blockage and other problems related to endometriosis.
Note that IVF can’t cure endometriosis. It can work around the complications the condition causes and improve your chances of a successful pregnancy.

Source: Matilda Wormwood
How does endometriosis affect fertility?
During each cycle, the lining of the uterus (endometrium) builds up in preparation for pregnancy. In a healthy cycle, this tissue is shed during menstruation. With endometriosis, tissue similar to the uterine lining grows in places it shouldn’t, such as outside the uterus, on the ovaries, within the fallopian tubes, or even on nearby organs.
This misplaced tissue has no means of leaving the body when it breaks down and bleeds. Over time, it can lead to the development of cysts, scar tissue, and chronic inflammation.
Here’s how these changes can influence fertility:
Anatomical changes: Scarring and adhesions may distort pelvic anatomy or block the fallopian tubes, preventing eggs and sperm from meeting.
Inflammation: Ongoing inflammation can reduce egg quality and create an inhospitable environment for sperm and embryos.
Ovarian reserve and stimulation response: Some studies show that women with endometriosis may have fewer eggs retrieved during IVF.
Implantation and miscarriage risk: There may be a slightly higher risk of implantation problems and miscarriage, though evidence is mixed and not always consistent.
How does endometriosis affect IVF?
Women with endometriosis may produce fewer eggs during stimulation, particularly if they have large endometriomas (ovarian cysts associated with endometriosis), but the retrieved eggs typically show preserved quality.
Rates of fertilization, embryo growth, and chromosomal health are not significantly different from those seen in other causes of infertility. This means that clinicians don’t have to default to more aggressive protocols, such as ICSI, solely because of endometriosis.
Additionally, the ability of the uterus to support implantation is not substantially reduced in most women with endometriosis.
Some fertility doctors may recommend therapy or surgery before IVF. Still, surgery to remove endometriomas is not always beneficial because it can damage the ovaries and reduce ovarian reserve without improving live birth rates. Surgery is only necessary to relieve symptoms or improve access to the ovaries during egg retrieval.
Before making such decisions, your doctor must assess:
Ovarian reserve
Tubal patency (openness of your fallopian tubes)
Uterine cavity
Overall, IVF protocols don’t need to be fundamentally different if you have endometriosis. What matters most is personalizing your treatment, taking into consideration:
Disease severity
Ovarian reserve
Previous fertility history
Can IVF cause endometriosis or make it worse?
There is no evidence suggesting that IVF can cause endometriosis. However, estrogen is the hormone primarily responsible for endometriosis, and IVF relies on estrogen during ovarian stimulation. If estrogen is given to a woman with endometriosis, the tissue may grow bigger and become inflamed, exaggerating the symptoms.

Source: Sora Shimazaki
Still, research on women with deep invasive endometriosis shows that IVF doesn’t increase the risk of disease progression or recurrence.
In a study of 84 women, only one possible endometriosis-related complication occurred, corresponding to a rate of 1–1.7%. Pain levels and lesion sizes remained stable throughout treatment. These numbers are similar to what is observed in women with endometriosis who don’t undergo IVF.
Another study confirms this finding, noting that IVF doesn’t seem to accelerate disease progression.
How does IVF work if you have endometriosis?
Doctors usually recommend trying to conceive naturally for up to a year if you’re under 35, or six months if you’re over 35, before diagnosing infertility. However, they may consider fertility treatment sooner if you have endometriosis, since the condition can reduce the chances of natural conception.
For people with endometriosis, the IVF process is essentially the same as it is for others. It begins with an initial consultation with a fertility specialist to discuss your medical history and undergo fertility testing so you can come up with a tailored treatment plan.
The initial step may also include an MRI or an ultrasound to assess the presence of endometriomas. Some clinics also include ovarian suppression in their protocols, which involves prescribing medications (e.g., GnRH agonists) before stimulation to reduce estrogen activity.
The following steps are the same for all prospective parents:
Step | What happens |
|---|---|
Ovarian stimulation |
|
Egg retrieval |
|
Fertilization |
|
Embryo culture |
|
Embryo transfer |
|
Luteal phase support |
|
About two weeks after transfer, a blood test is performed to check for pregnancy. If successful, early monitoring continues. If not, your doctor may adjust protocols or transfer one of the remaining frozen embryos in a later cycle.
💗 Pro tip!
Embryo grading evaluates the appearance of embryos under a microscope. Preimplantation genetic testing (PGT-A, PGT-M, PGT-SR, and PGT-P) looks at the chromosomal health of each embryo, helping you and your doctor choose the one with the highest likelihood of healthy development.
For parents with endometriosis, where implantation can be more challenging, PGT offers additional reassurance.
Bonus read: Understand IVF genetic testing better, and explore its benefits and potential risks in these guides:

Can endometriosis affect IVF success?
The impact of endometriosis on IVF outcomes has been studied extensively, but results remain mixed. Some studies show little difference in success rates between people with endometriosis and those with other causes of infertility. Other studies indicate that endometriosis can lower the chances of pregnancy, particularly in untreated or severe cases.
A 2021 study of 330 participants concluded that treating endometriosis before IVF significantly improves outcomes. Here’s what it found:
Untreated endometriosis | Early-treated endometriosis | Late-treated endometriosis |
|---|---|---|
|
|
|
A 2012 study found that the severity and stage of the condition play critical roles in IVF outcomes. It demonstrated that deeply infiltrative endometriosis lowers IVF success, whereas mild or superficial disease has a moderate effect.
Patients with severe endometriosis had lower pregnancy rates, fewer eggs retrieved, decreased fertilization rates, and lower implantation rates. These results suggest that endometriosis can impact egg and embryo development, not only the uterine environment.
Depending on the stage of endometriosis, the success rates are:
Stage I or II: About 67.7% after one to four IVF cycles
Stage III or IV: About 56.7% after one to four IVF cycles
IVF can be effective for people with endometriosis, but outcomes vary depending on many different factors. That’s why personalized care, advanced genetic insights, and ongoing professional guidance are essential throughout the fertility journey.
Tailoring treatment to your unique situation, from assessing parental DNA to selecting the optimal embryo for transfer, can significantly improve success rates. Nucleus IVF+ offers a comprehensive, all-in-one solution, designed to support you at every stage of your IVF experience, improving your chances of success with every step. You can sign up here.
How Nucleus IVF+ optimizes IVF success
Nucleus IVF+ is the first IVF program that combines advanced genetic optimization with human-centered care. You don’t have to piece together multiple tests and services because Nucleus provides a complete, concierge-style package that includes clinical, genetic, and personalized support.
With Nucleus IVF+, you gain access to the fertility support unique to your case. We’ll help you choose a clinic that meets your medical and personal needs, and if necessary, a genetically compatible donor.
The package includes a complete IVF cycle, with medications, ICSI, lab work, and unlimited consultations with genetic counselors throughout your treatment. It also integrates Nucleus’s three core products:
Nucleus Preview: Comprehensive carrier screening for both parents, for 2,000+ genetic conditions you could pass on to your child.
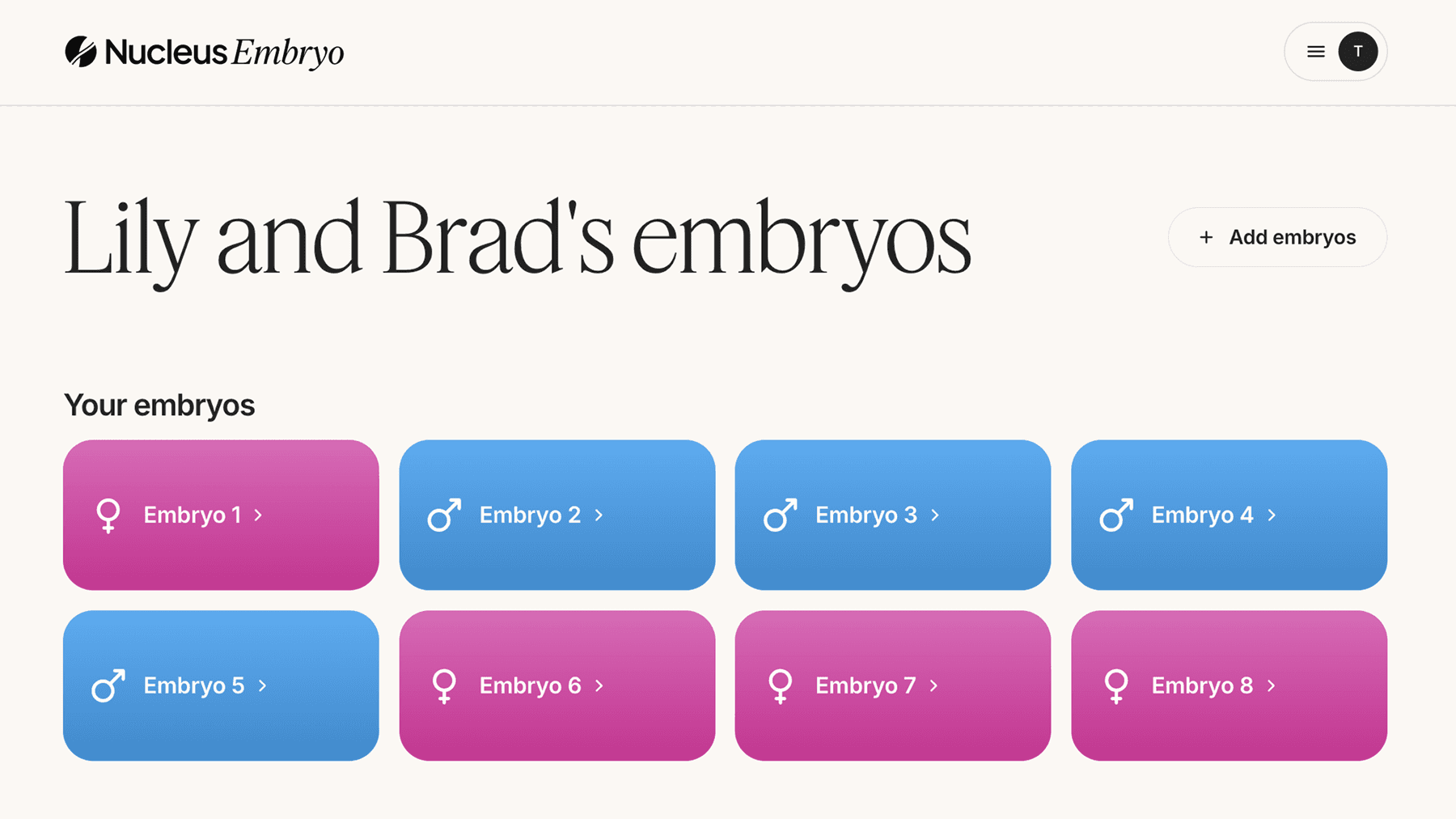
Nucleus Embryo: Advanced software that helps you compare embryos side-by-side in an interactive dashboard and sort up to 20 embryos by health insights, well-being traits, and more.
Nucleus Health: Personalized health reports, highlighting lifestyle adjustments, risk factors, and actionable steps to improve your health.

Every aspect of your fertility journey is streamlined and personalized, maximizing your chances of success.
Schedule a call with Nucleus today and talk to our experts.
You may also like…
Featured image source: Andrea Piacquadio












