Tubal ligation is a surgical procedure that blocks the fallopian tubes to prevent pregnancy and reduce the risk of ovarian cancer. It’s a permanent form of birth control, but many women reconsider later due to evolving life circumstances, such as a new relationship or a desire for more children.
Natural conception isn’t an option after tubes have been tied, but modern fertility treatments offer a solution.
To explain what your options are after tubal ligation, we’ll answer the following questions:
Can you do IVF if your tubes are tied?
How does IVF work after tubal ligation?
How much is IVF after a tubal ligation?
How successful is IVF after tubal ligation?
Can you do IVF after a tubal ligation?
Yes, you can do IVF with your tubes tied.
Tubal ligation prevents sperm from traveling to the fallopian tubes and meeting the eggs released from the ovaries. Even if you ovulate and sperm are present, natural fertilization can’t happen.
Surgeons may use different methods, such as:
Clipping
Banding
Clamping
Cauterizing
Removing part of the tubes
However, IVF doesn’t depend on the fallopian tubes. Instead of waiting for eggs to travel down the tubes, doctors retrieve them directly from the ovaries. The eggs are fertilized with sperm in the lab. Once the embryos develop, one (sometimes more) is placed directly into the uterus, completely bypassing the fallopian tubes.

Source: Samuel Nuñez
If you decide to have a baby after tubal ligation, you can also have the reversal surgery. It may allow you to conceive naturally or through simpler, less expensive procedures, such as intrauterine insemination. However, it’s another major procedure that requires hospitalization and recovery, and like all surgical procedures, it carries risks, so IVF may be a safer solution.
IVF vs. reversal surgery
Tubal ligation reversal surgery (tubal anastomosis) reconnects the previously cut or blocked fallopian tubes to enable natural conception. The success of the procedure depends on several factors, including:
Type of tubal ligation performed: Methods like clipping have higher reversal success because most of the tube is saved, and it can be reconnected more easily.
Lengths and condition of the remaining tubal segments: Longer, healthier remaining tubal stumps and intact fimbria (ends that pick up eggs from the ovary) improve your chances.
Maternal age: Women under 35 have the best outcomes, with pregnancy rates after reversal up to 75% if all factors are favorable. Success declines gradually in the late 30s and drops sharply after 38. IVF is a better solution for older women, while reversal may be recommended to women under 35.
Egg quantity and quality: Even if the tubes are successfully reconnected, low ovarian reserve or poor egg quality can limit pregnancy chances.
Presence of other pelvic conditions: Endometriosis, scar tissue, or adhesions around the ovaries or tubes can interfere with natural conception after reversal surgery.
Sperm quality: Low sperm count, poor motility, or abnormal morphology may make natural conception after reversal unlikely. IVF with ICSI can overcome this.
Here’s a side-by-side comparison of IVF and reversal surgery:
Factor | IVF | Tubal reversal surgery |
|---|---|---|
Invasiveness |
|
|
Time to pregnancy |
|
|
Risks |
|
|
Can you do IVF if your tubes are removed?
Yes, you can do IVF after tubal removal.
Unlike tubal ligation, where the tubes are tied or blocked but remain in the body, in tubal removal or bilateral salpingectomy, both tubes are surgically removed.
Your doctor may recommend tubal removal due to medical conditions such as:
Risk of ovarian cancer: 70% of the most frequent ovarian cancers begin in the fallopian tubes
Ectopic pregnancy: When an embryo implants in the fallopian tube instead of the uterus
Hydrosalpinx: Fluid-filled, damaged tubes that can leak into the uterus and interfere with implantation
Endometriosis: When abnormal tissue growth damages the tubes
Infection or scarring: Leading to non-functional or harmful tubes
If your tubes have been previously damaged or infected, IVF can even be more successful after tubal removal because it eliminates risks and may improve pregnancy rates.

Source: Isaac Taylor
How long after tube removal can you start IVF?
The recovery time after tube removal is usually short (2–4 weeks), and most people can start IVF as soon as they heal from the surgery and their doctor confirms that their ovaries and uterus are healthy.
Real-life experiences show that the timeline is often a matter of weeks to a few months. For example, one Redditor had a frozen embryo transfer less than six weeks after surgery. Another mom did stimulation and retrieval before the surgery, so the process is as short as possible:
Good to know! 🤎
Whether you’ve had your tubes tied or completely removed, as long as your ovaries produce eggs and your uterus can support the pregnancy, you can have a baby through IVF.
In fact, even if your ovaries aren’t working well due to a medical reason or if you’re in perimenopause or menopause, you can still get pregnant with IVF using donor eggs.
How does IVF work after tubal ligation?
Blocked fallopian tubes don’t affect the core IVF steps. Here’s how the process works:
Ovarian stimulation: Fertility medications encourage the ovaries to produce multiple eggs in one cycle instead of the single egg released during natural ovulation. More eggs mean more chances of creating healthy embryos.
Monitoring and timing: Ultrasounds and blood tests track the development of the follicles. When the eggs are mature, a trigger shot is given to prepare them for retrieval.
Egg retrieval: Using a thin needle guided by ultrasound, your fertility doctor collects eggs directly from the ovaries. It is a short outpatient procedure usually done under light sedation.
Fertilization: Retrieved eggs are fertilized with sperm in a controlled lab environment, either by letting them combine naturally in a dish or by injecting a single sperm directly into an egg through intracytoplasmic sperm injection (ICSI).
Embryo development: Over the next few days, fertilized eggs develop into embryos. Embryologists carefully monitor their growth and grade them to help identify the healthiest ones. Once embryos reach the blastocyst stage (day 5 or 6), they undergo preimplantation genetic testing.
Embryo selection: While you wait for embryo genetic testing results (1–6 weeks), your embryos are frozen and safely stored. You will then select the healthiest embryo with the best chances of implantation and successful pregnancy.
Embryo transfer: The chosen embryo is placed directly into the uterus using a thin catheter. Since the embryo doesn’t need to travel through the fallopian tubes, their condition does not affect this step. Many clinics perform a mock transfer to anticipate potential issues and determine the best transfer technique.
Pregnancy test: After approximately two weeks, the beta-hCG blood test will indicate whether implantation was successful. If the initial test is positive, the test is repeated. hCG levels should double and continue rising. Two weeks later, an ultrasound will confirm an intrauterine pregnancy.
Embryo selection in IVF after tubal ligation
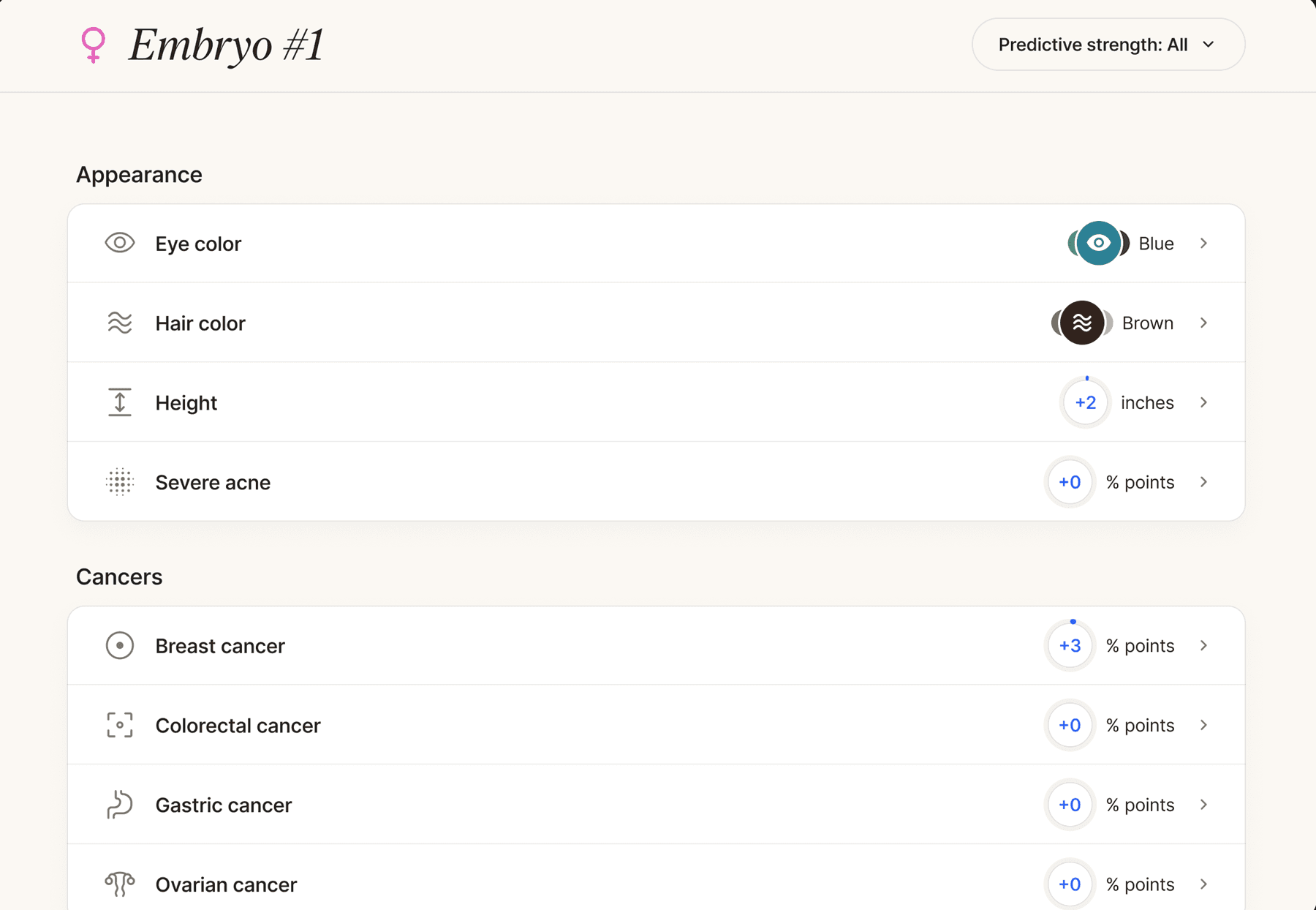
Regardless of tubal ligation, standard genetic testing options help identify embryos most likely to implant and develop normally. More advanced tests, such as polygenic embryo screening, look beyond viability and provide information about the potential long-term health and well-being of your future child.
Here’s an overview of the embryo testing options available:
Test type | What it does |
|---|---|
Screens embryos for abnormal numbers of chromosomes (also reveals the sex, if relevant for sex-related genetic conditions) | |
Detects single-gene disorders when parents are known carriers, preventing genetic conditions such as cystic fibrosis and hemophilia | |
Identifies chromosomal translocations or structural issues in embryos | |
Advanced testing method that screens embryos for chronic, adult-onset conditions, such as heart disease and diabetes |
How much is IVF after a tubal ligation?
Tubal ligation has no impact on the cost of IVF. On average, one IVF cycle can cost from $15,000 to $30,000, but the final price will depend on:
Your location
Clinic fees
Your protocols
Whether you need donor eggs or sperm
Additional services, such as embryo storage, genetic testing, and ICSI
The number of cycles necessary
Depending on your policy, your insurance may cover some parts of the treatment.
Reversal surgery costs vary depending on the surgeon and hospital, and can range from $3,000 to $8,000 for physician fees and from $7,000 to $20,000 for hospital and anesthesia charges.
How successful is IVF after tubal ligation?
A 2015 study found that tubal ligation doesn’t directly affect IVF success, which primarily depends on your age, egg quality, sperm quality, and overall uterine health.
The most accurate predictor of IVF success is maternal age because the quality and quantity of eggs decline over time. Older eggs are more prone to genetic abnormalities, which can lead to failed implantation or early miscarriage.

Source: RDNE stock project
Still, studies comparing IVF with tubal ligation reversal show some interesting findings. In one study, 31 women underwent IVF, and 12 underwent reversal surgery. Pregnancy rates were higher with tubal reversal (75% vs. 35.5%), and live birth rates were also higher (58.3% vs. 25.8%).
In the same study, 68% of participants preferred surgery to IVF, but many changed their minds after learning more about the procedure, so 54.6% favored IVF. That demonstrates how informed counseling can aid in making smart decisions.
Deciding to do IVF when tubes are tied is a huge medical, financial, and emotional step. Although the procedure bypasses the tubes, removes the need for a major surgery, and has strong success rates, many parents still struggle with questions about choosing the right IVF clinic, accessing genetic testing, or finding appropriate support along the way.
Nucleus IVF+ provides comprehensive, personalized guidance from the moment you decide to pursue IVF to make the journey smoother and clearer.
Start exploring Nucleus support options here.
A streamlined path to parenthood with Nucleus IVF+
Today, families choose IVF for more than overcoming fertility challenges. They want clarity, empowerment, and the ability to make informed choices about their future children. Nucleus IVF+ goes beyond viability, offering advanced genetic insights, personalized guidance, and comprehensive features that can help you grow your family with confidence.
From selecting the right clinic and donor to understanding embryo health, Nucleus IVF+ empowers every parent to make informed, data-driven decisions at every step.
Clinic matching: You work with a team that has proven success rates tailored to your medical and personal needs.
Nucleus Health DNA testing: Receive reports that help you take proactive steps for your own long-term health and longevity.
Donor selection: You choose someone who matches your family goals and is genetically compatible with you.
Personalized genetic insights: After preconception screening with Nucleus Preview, we explain your carrier status and risks you may pass on to your child.
In-depth embryo analysis: Nucleus Embryo AI-powered analysis tool provides comprehensive information about your embryos’ genetic makeup, helping you compare and choose based on long-term health and well-being markers.
Start your journey by booking an onboarding call with the Nucleus team to find optimal solutions. We guide you with 24/7 compassionate support and unlimited access to genetic counselors.
Featured image source: Dhemer Gonçalves












